Treatment for Osteoporosis: The 5 Exercise Benefits You Need
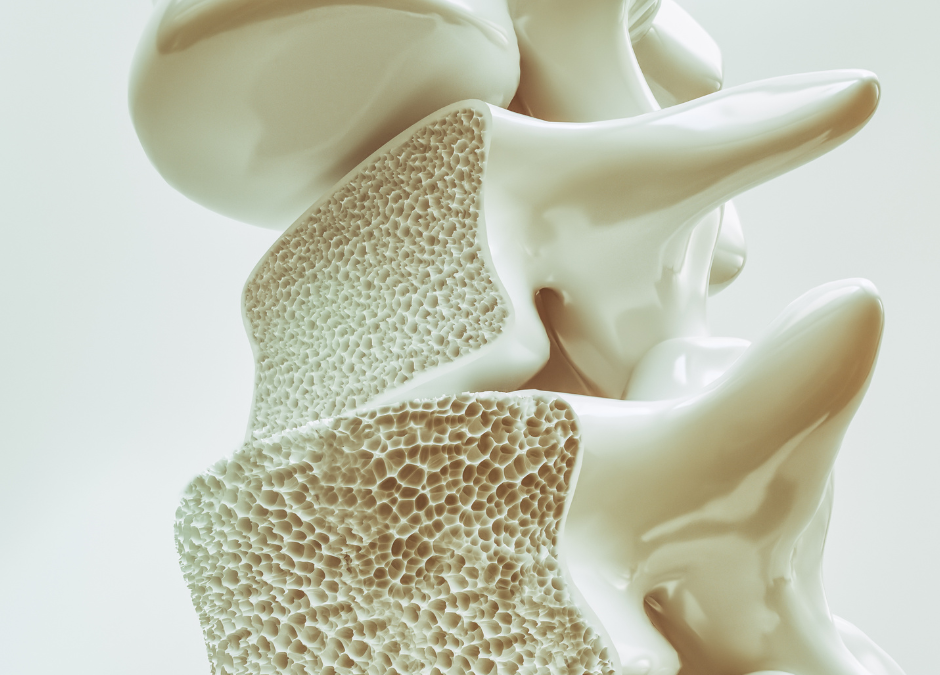
Osteoporosis is a prevalent and serious health concern that affects millions of people globally, particularly older adults. This condition, characterised by weakened and brittle bones, significantly increases the risk of fractures, which can lead to a decline in overall quality of life. Early diagnosis, effective treatment for osteoporosis, and proactive prevention strategies are essential to manage the condition and minimise the risk of complications.
This blog will explore the causes, prevention, management, and options of treatment for osteoporosis, with a special focus on the critical role of exercise that is normally overlooked when treatment plans are put together.
What is Osteoporosis?
Osteoporosis is a condition that results in decreased bone density and mass, making bones fragile and more prone to fractures. Even minor falls or, in severe cases, everyday actions like bending over or coughing can lead to bone fractures. The hips, spine, and wrists are the most common sites for osteoporosis-related fractures.
While anyone can develop osteoporosis, the condition is particularly prevalent among postmenopausal women, elderly men, and individuals with a genetic predisposition. However, it is important to note that osteoporosis is not an inevitable consequence of ageing. With the appropriate prevention, lifestyle changes, and treatment for osteoporosis, the onset of the condition can be delayed or even prevented.
Causes of Osteoporosis

Understanding it’s causes is crucial for the prevention, management and treatment for osteoporosis. Several factors can contribute to it’s development:
1. hormonal changes
Hormonal changes, particularly in women, are one of the primary causes of osteoporosis. Estrogen, a hormone that plays a key role in maintaining bone density, significantly decreases after menopause, accelerating bone loss. Men also experience a gradual decline in testosterone, which can contribute to bone weakening over time.
2. ageing
Bone density naturally decreases with age. As we grow older, the body’s ability to regenerate new bone tissue diminishes, leading to a gradual reduction in bone mass. Without preventive measures, this process can result in osteoporosis.
3. genetic factors
Genetics also play a significant role in an individual’s bone density and risk of developing osteoporosis. A family history of osteoporosis can increase the likelihood of developing the condition, as certain genetic markers associated with bone density regulation have been identified.
4. Nutritional Deficiencies
Adequate intake of calcium and vitamin D is essential for maintaining strong bones. Calcium serves as a fundamental building block for bone tissue, while vitamin D helps the body absorb calcium effectively. Deficiencies in these nutrients can lead to weakened bones and a higher risk of osteoporosis.
5. lifestyle factors
Certain lifestyle choices can significantly increase the risk of developing osteoporosis:
- physical inactivity:
A sedentary lifestyle contributes to bone loss. Weight-bearing exercises, such as walking, jogging, and resistance training, are vital for maintaining bone density.
- Smoking and Excessive Alcohol Consumption:
Smoking impairs the body’s ability to absorb calcium, and excessive alcohol intake can interfere with bone formation, increasing the risk of fractures.
6. Medical Conditions and Medications
Some medical conditions, like rheumatoid arthritis, thyroid disorders, and celiac disease, can increase the risk of osteoporosis. Long-term use of corticosteroids, commonly prescribed for inflammatory conditions, can also lead to significant bone loss.

5 strategies to Prevent the need of treatment for osteoporosis
Preventing osteoporosis is more effective than treating it after it has developed. Several strategies can help reduce the risk of developing osteoporosis:
1. Nutrition
Maintaining a diet rich in calcium and vitamin D is crucial for bone health. Dairy products, leafy green vegetables, and fortified foods are excellent sources of calcium. Vitamin D can be obtained from sunlight exposure and dietary sources like fatty fish and fortified foods. In some cases, supplements may be necessary to meet daily requirements.
2. Regular Exercise
Exercise is one of the most effective ways to prevent osteoporosis. Engaging in regular physical activity, particularly weight-bearing exercises like walking, jogging, and resistance training, strengthens bones and stimulates bone formation. These activities create stress on the bones, encouraging them to increase density and remain strong. Additionally, exercises that improve balance and flexibility, such as yoga and tai chi, can reduce the risk of falls, thereby preventing fractures.
3. lifestyle modifications
Avoiding smoking and limiting alcohol intake are vital steps in maintaining bone health. Both smoking and excessive alcohol consumption are linked to increased bone loss and higher fracture risks.

4. Bone density testing
Regular bone density testing, particularly for postmenopausal women and older adults, can help detect osteoporosis early. The dual-energy X-ray absorptiometry (DEXA) scan is the most common test used to measure bone density and assess fracture risk.
5. Medications
In some cases, preventive medications may be prescribed to individuals at high risk of osteoporosis. These medications, which will be discussed in more detail in the treatment section, can help maintain bone density and prevent fractures.
The Importance of Exercise in Prevention and Management
Exercise plays a dual role in both the prevention and management of osteoporosis. It not only helps to prevent the onset of osteoporosis but also plays a critical role in managing the condition in those who have already been diagnosed.

1. Bone Strengthening
Weight-bearing and resistance exercises are particularly beneficial for bone health. Activities such as walking, running, dancing, and weightlifting create mechanical stress on bones, which stimulates bone-forming cells known as osteoblasts. This process leads to the formation of new bone tissue, increasing bone density and strength.
2. Muscle Strength and Balance Improvement
Exercises that enhance muscle strength and balance are crucial for preventing falls, which is a primary concern for individuals with osteoporosis. Strengthening the muscles around the bones, particularly in the hips, back, and legs, provides better support and reduces the likelihood of fractures from falls. Balance-focused exercises, such as tai chi and yoga, further enhance stability, making falls less likely.
3. Posture and Spine Health
Osteoporosis often affects the spine, leading to a stooped posture or even vertebral fractures. Exercises that improve posture, strengthen the back muscles, and enhance flexibility can alleviate pressure on the spine, reduce pain, and prevent further bone deterioration.
4. Enhanced Mobility and Quality of Life
Regular physical activity improves overall mobility and flexibility, which are often compromised in individuals with osteoporosis. By maintaining an active lifestyle, people with osteoporosis can preserve their independence and quality of life, reducing the impact of the condition on their daily activities.
5. mental health benefits
Beyond the physical benefits, regular exercise also has positive effects on mental health. It can help reduce anxiety, depression, and the stress associated with living with a chronic condition like osteoporosis. Improved mental well-being can lead to better adherence to treatment plans and a more proactive approach to managing the condition.
Management & Treatment of Osteoporosis
For those diagnosed with osteoporosis, managing the condition involves a combination of lifestyle changes, medication, and regular monitoring. Effective management can slow the progression of the disease, reduce the risk of fractures, and improve quality of life.
1. Dietary Adjustments
As previously mentioned, a diet rich in calcium and vitamin D is crucial for managing osteoporosis. In addition to these nutrients, ensuring an adequate intake of protein is important, as it plays a role in bone repair and maintenance. Incorporating foods high in magnesium, potassium, and vitamin K can also support bone health.
2. Exercise Regimen
Exercise remains a cornerstone in managing osteoporosis. Weight-bearing exercises, like walking and dancing, and resistance training help maintain bone density. Additionally, balance and flexibility exercises, such as yoga and tai chi, can reduce the risk of falls by improving stability and coordination.
3. Fall Prevention Strategies
For individuals with osteoporosis, preventing falls is essential to avoid fractures. Some strategies include:
- Home Safety Modifications:
Removing tripping hazards, using non-slip mats, and installing grab bars in bathrooms can make the home environment safer.
- Vision and Hearing Checks:
Regular vision and hearing exams can help address issues that might contribute to falls.
- Proper Footwear:
Wearing supportive shoes with non-slip soles can reduce the risk of slipping.
4. regular monitoring
Individuals with osteoporosis should undergo regular bone density tests to monitor the effectiveness of their treatment plan. These tests can help assess whether bone density is being maintained or improving and whether any adjustments to treatment are necessary.
5. medication management
Several medications are available to treat osteoporosis, each with different mechanisms of action. The choice of treatment depends on the severity of the condition, the patient’s overall health, and other factors.
1. Bisphosphonates
Bisphosphonates are the most commonly prescribed medications for osteoporosis. They work by slowing down the rate at which bone is broken down in the body, allowing bone density to be maintained or even increased. Common bisphosphonates include:
– Alendronate (Fosamax)
– Risedronate (Actonel)
– Ibandronate (Boniva)
– Zoledronic acid (Reclast)
These medications are usually taken orally or administered via injection, with dosing schedules ranging from daily to yearly.
2. Selective Estrogen Receptor Modulators (SERMs)
SERMs, such as raloxifene (Evista), mimic the effects of estrogen in maintaining bone density. They are particularly beneficial for postmenopausal women and can reduce the risk of spine fractures. However, they may not be as effective as bisphosphonates in preventing hip fractures.
3. Hormone Replacement Therapy (HRT)
HRT involves the administration of estrogen, sometimes combined with progesterone, to help maintain bone density in postmenopausal women. However, HRT is associated with some risks and is generally considered when other treatment options are unsuitable.
In Summary: Causes, Prevention & Treatment For osteoporosis
Osteoporosis is a condition that requires proactive management, and understanding its causes, prevention, and treatment options is key to maintaining bone health. Early diagnosis, lifestyle changes, and effective treatment plans, including medication and exercise, can significantly reduce the risk of fractures and improve quality of life.
Exercise, in particular, plays a vital role in both preventing and managing osteoporosis. It strengthens bones, improves muscle mass and balance, and reduces the likelihood of falls, making it an often-overlooked but essential component of any osteoporosis treatment plan. By combining regular physical activity with proper nutrition, medical management, and lifestyle modifications, individuals can take control of their bone health and live a fuller, healthier life despite an osteoporosis diagnosis.
If you wish to seek further help or speak to a practitioner about any of the above, call us on 0800 731 2738 or book online here.
You can also view all the services we provide within our clinics on our website, as well as checking out our other blogs and content.
For more free tips and information, make sure to follow our Facebook and Instagram pages. We also post client stories, so you can see how we’ve helped people get back to doing the things they enjoy!