Heel pain when walking: 5 likely causes
Heel pain is a common complaint among many people, especially those who spend a lot of time on their feet. Whether you're an avid runner, a retail worker, or simply someone who enjoys long walks, heel pain can significantly affect your quality of life. Understanding the causes, treatment options, and preventive measures for heel pain when walking can help you to manage this discomfort and maintain an active lifestyle.
common causes of heel pain when walking
Heel pain can stem from various conditions, each with distinct causes and characteristics. Here are some of the most common causes:
1. plantar fasciitis
Plantar fasciitis is one of the most prevalent causes of heel pain. It occurs when the plantar fascia, a thick band of tissue that runs across the bottom of your foot and connects your heel bone to your toes, becomes inflamed. This condition often results from repetitive strain or overuse, such as from running, walking long distances, or standing for extended periods.
Symptoms:
- Sharp pain in the heel, particularly with the first steps in the morning or after periods of rest.
- Pain that improves with movement but worsens after prolonged activity.

2. Heel Spurs
Heel spurs are bony growths that develop on the underside of the heel bone. They are often associated with plantar fasciitis, though not all individuals with heel spurs experience pain. These spurs can cause discomfort by irritating the surrounding tissues.
symptoms:
- Pain similar to plantar fasciitis, often described as a stabbing sensation.
- Pain may worsen with activity and improve with rest.
3. achilles tendinitis
Achilles tendinitis involves inflammation and degeneration of the Achilles tendon, which connects the calf muscles to the heel bone. This condition is typically caused by overuse or repetitive stress, especially in athletes or individuals who suddenly increase their activity levels.
symptoms:
- Pain and stiffness along the Achilles tendon, especially in the morning.
- Swelling and tenderness at the back of the heel.
4. Bursitis
Bursitis occurs when the bursae, small fluid-filled sacs that cushion the bones, tendons, and muscles near the joints, become inflamed. In the heel, this inflammation often affects the retrocalcaneal bursa, located between the Achilles tendon and the heel bone.
symptoms:
- Pain and swelling at the back of the heel.
- Tenderness and discomfort, especially when pressing on the affected area.

5. stress fractures
Stress fractures are tiny cracks in the bone, often caused by overuse or repetitive impact. In the heel, these fractures can develop from activities like running, jumping, or marching.
symptoms:
- Gradual onset of pain that worsens with weight-bearing activities.
- Localised tenderness and swelling.
Diagnosing the cause of your heel pain
Diagnosing the underlying cause of heel pain involves a combination of physical examination, medical history, and sometimes imaging tests. Here’s what you can expect during a diagnosis:
medical history
Your practitioner will ask about your symptoms, activity levels, and any recent injuries or changes in your routine.
physical examination
Your practitioner will examine your foot, checking for areas of tenderness, swelling, and range of motion. They may also observe your gait and posture.
Onward referral/Imaging
X-rays, MRI, or ultrasound may be used if needed to get a detailed view of the structures within the foot and identify conditions like heel spurs, stress fractures, or soft tissue inflammation.
treatment options for those experiencing heel pain when walking
Treatment for heel pain varies based on the underlying cause but generally includes a combination of home care, medical treatments, and lifestyle modifications.
home care
1.rest and ice
Resting the affected foot and applying ice packs can help reduce inflammation and relieve pain. Ice should be applied for 15-20 minutes several times a day.
2. stretching exercises
Stretching the plantar fascia, Achilles tendon, and calf muscles can improve flexibility and reduce tension on the heel. Simple exercises include calf stretches, towel stretches, and rolling a tennis ball under the foot.

3. Footwear
Wearing supportive shoes with proper arch support and cushioning can alleviate pressure on the heel. Avoid high heels and opt for shoes designed for your specific activity, whether running, walking, or standing.
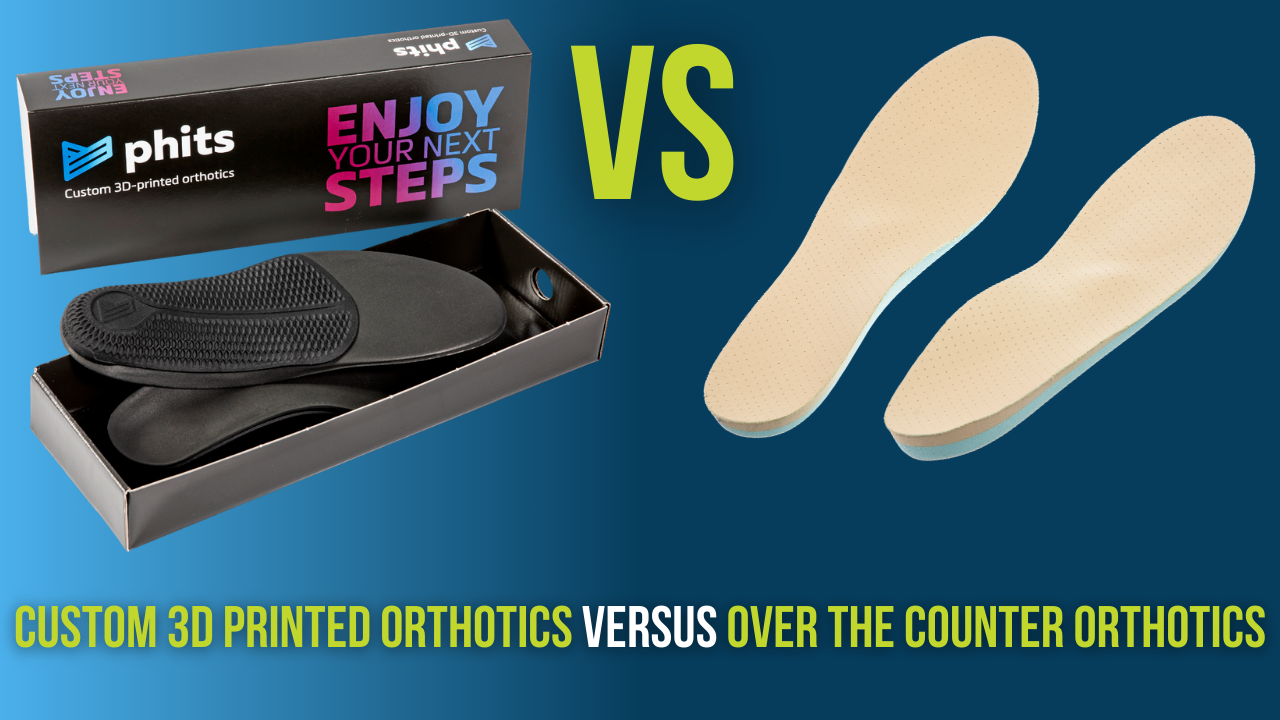
4. orthotics
Over-the-counter or custom orthotic inserts can provide additional support and cushioning, helping to distribute pressure more evenly across the foot. Here at Summit, we offer state of the art gait analysis, from this analysis we are given custom data from the scans, meaning we can then produce a pair of custom 3D printed orthotics that are designed specifically for your feet.
medical treatments
1. physical therapy
A physical therapist can develop a personalised exercise and stretching program to address the specific cause of your heel pain. They may also use techniques like ultrasound therapy or manual manipulation to promote healing.
2. medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can help reduce pain and inflammation. Your doctor may also prescribe stronger medications if necessary.
3. Corticosteroid Injections
In cases of severe pain, corticosteroid injections can provide temporary relief by reducing inflammation in the affected area.
4. ShockWave Therapy
Extracorporeal Shockwave Therapy (ESWT) is a non-invasive treatment that uses sound waves to stimulate healing in the plantar fascia and other soft tissues. It is often used when conservative treatments fail to provide relief.
5. surgery
In rare cases where other treatments are ineffective, surgical intervention may be necessary. Procedures can include releasing the plantar fascia, removing heel spurs, or repairing damaged tendons.

Preventing Heel Pain when walking
Preventing heel pain involves adopting habits and practices that reduce the risk of injury and strain on the feet. Here are some preventive measures:
1. wear proper footwear
Invest in shoes that provide adequate support, cushioning, and fit well. Replace worn-out shoes regularly, and choose footwear appropriate for your activities.
2. gradual activity increase
Avoid sudden increases in physical activity. Gradually build up the intensity and duration of exercise to allow your body to adapt.
3. stretching & strengthening
Incorporate regular stretching and strengthening exercises into your routine. Focus on the plantar fascia, Achilles tendon, and calf muscles to maintain flexibility and strength.

4. maintain a healthy weight
Excess weight puts additional stress on the feet, increasing the risk of heel pain. Maintain a healthy weight through a balanced diet and regular exercise.
5. use the correct techniques
Whether running, walking, or standing, use proper techniques to minimise strain on your feet. Consider consulting you clinician for guidance on proper form.
6. rest & recovery
Allow adequate time for rest and recovery between intense physical activities. Overtraining can lead to overuse injuries like plantar fasciitis and Achilles tendinitis.
when to seek advice
While experiencing mild heel pain when walking can often be managed with home care and preventive measures, it’s important to seek medical attention if:
- Pain persists or worsens despite home treatment.
- You experience severe pain or swelling.
- You have difficulty walking or bearing weight on the affected foot.
- There is noticeable redness, warmth, or other signs of infection.
- Pain is accompanied by a fever.
A healthcare professional can provide a proper diagnosis, recommend appropriate treatments, and help you develop a plan to manage and prevent heel pain.
in Conclusion...
Heel pain when walking can be a debilitating condition that affects your daily activities and overall well-being. Understanding the causes, treatment options, and preventive measures can empower you to take control of your foot health. By addressing the underlying issues, making informed choices about footwear and activity levels, and seeking professional care when needed, you can reduce your risk of heel pain and maintain an active, pain-free lifestyle.
If you wish to seek further help or speak to a practitioner about any of the above, call us on 0800 731 2738 or book online here.
You can also view all the services we provide within our clinics on our website, as well as checking out our other blogs and content.
For more free tips and information, make sure to follow our Facebook and Instagram pages. We also post client stories, so you can see how we’ve helped people get back to doing the things they enjoy!