The Patellar Tendon
If we’re going to talk about patellar tendinitis, it’s probably a good idea to start by answering the question; what is the patellar tendon?
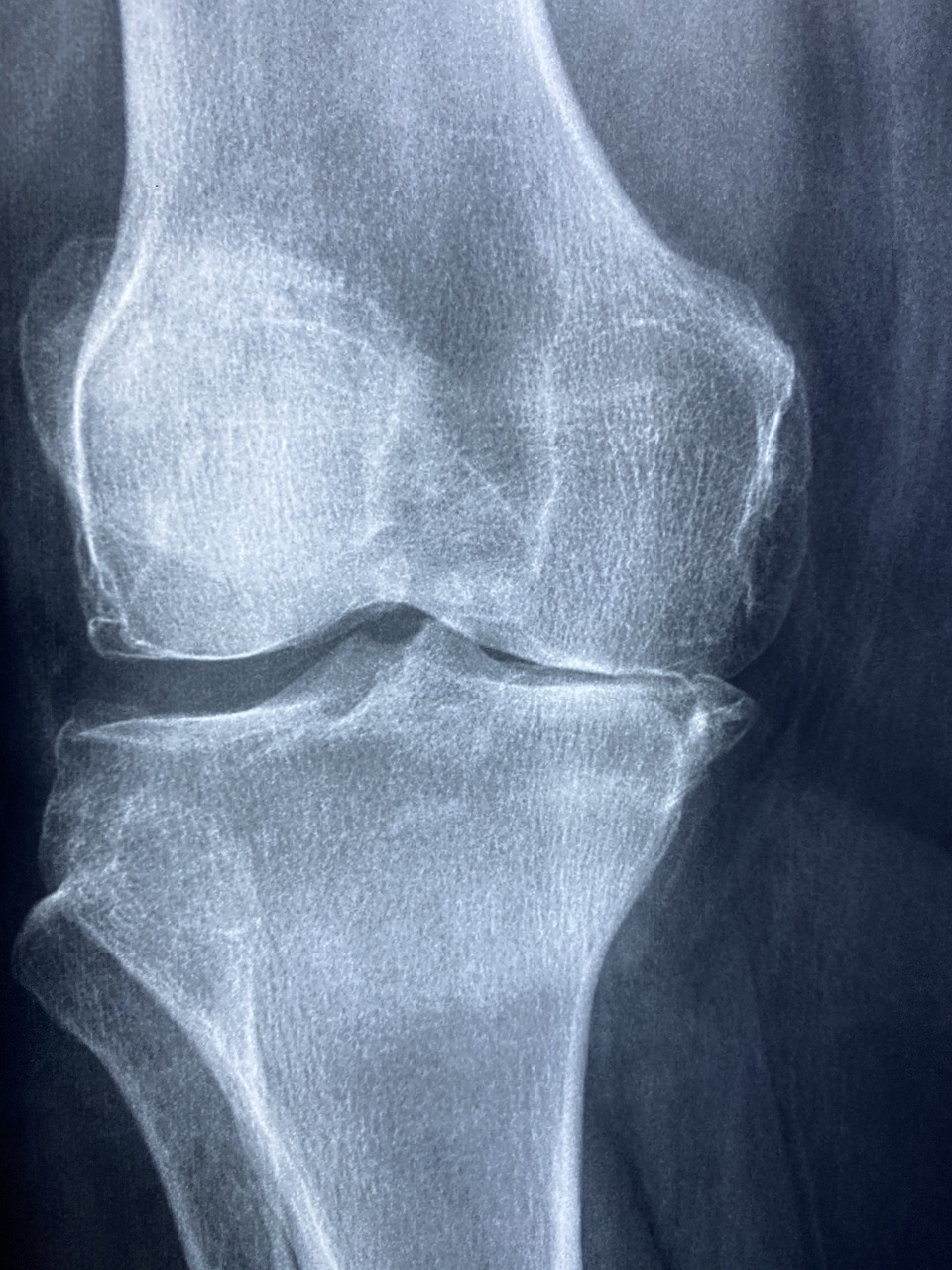
A tendon Is a piece of connective tissue connecting muscle to bone, tendons are structurally different to muscles as they are made largely of collagen fibres and are unable to contract. The patellar tendon is a tendon approximately 5ish cm in length and encases the patella (kneecap).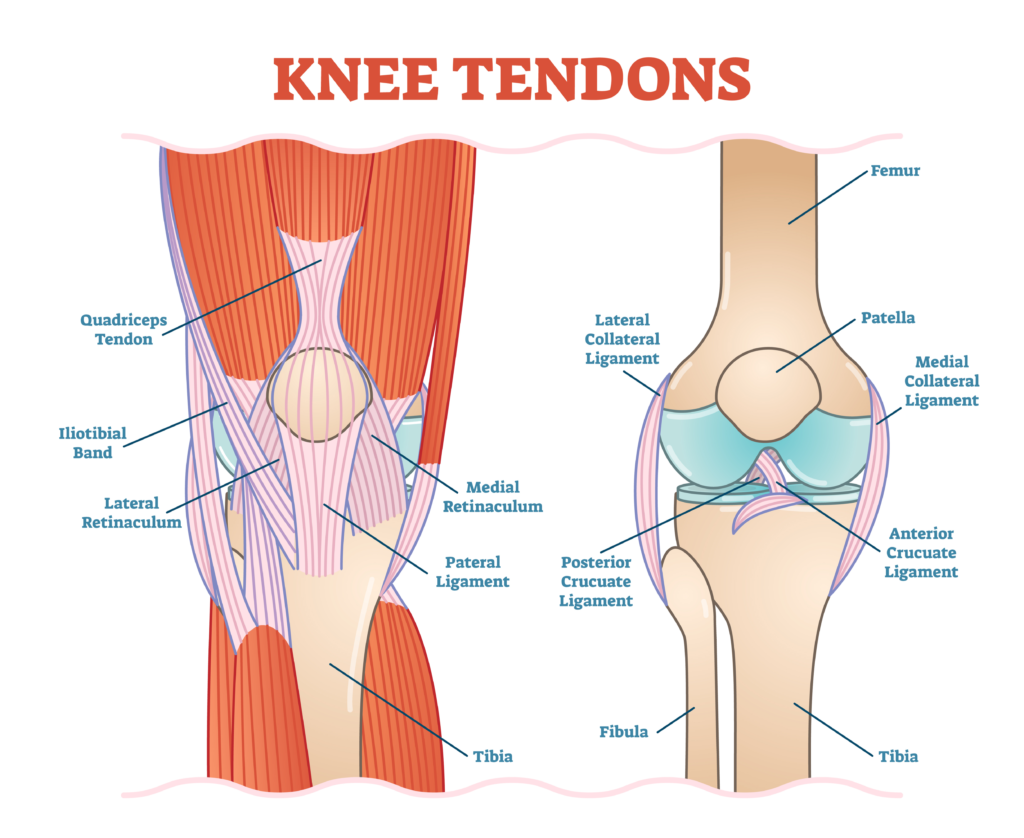
The patellar tendon is different to most tendons not only because the kneecap sits within it but also because this tendon connects bone to bone much like a ligament. It begins at the patella apex (on the end of the thigh bone) and inserts at the tibial tuberosity (the nobbly bit between your shin and knee.)
The patellar tendon is attached at the top to the quadriceps muscles, which shorten and pull the kneecap upwards.
The patella tendon and the thigh bone are separated by a spongy fat pad, the tendon and the shin bone are separated by a bursa (sack of fluid). Both structures can become irritated by patellar tendinitis or are often misdiagnosed as patellar tendinitis.
What does the Patellar Tendon do?
All tendons play a vital role in storing and releasing energy to help you move, they act a bit like springs in that when you apply load to them they have a recoil mechanism to make your movements more efficient and require less effort. The patella tendon does this for things like sprinting and jumping
The Patella plays an important role in the mechanics of the knee. It sits in a groove and slides up when the knee is straightening and drops down as the knee bends and the Patella tendon effectively lengthens.
As the patella tendon is shortened by the quads it pulls the shin bone upwards in order to straighten the knee, similarly to a pulley system in order to lift something heavy.
What is Patellar Tendinitis?
 Whenever you see anything medical with the suffix ‘itis’ it means inflammation, for that reason patellar tendinitis describes inflammation at the patella tendon.
Whenever you see anything medical with the suffix ‘itis’ it means inflammation, for that reason patellar tendinitis describes inflammation at the patella tendon.
If you ever have a scan or a conversation with a medical professional it is more likely you will be told you have a patellar tendinopathy.
Patellar tendinopathy has historically been thought of as an inflammatory condition as a result of persistent microtraumas. However, recent studies suggest that tendinopathies can show pain with the absence of inflammation. Therefore, there is likely to be an inflammatory component at some stage but it makes more sense to divide these conditions into 3 categories and place them on a continuum (sliding scale):
Reactive tendinopathy
In this phase not much happens to the structural integrity of the tendon, although images have shown that there are bits of tendon thickening at the specific areas which are being overloaded. Within the cells that make up to the tendon there is thought to be an overproduction of ‘Hydrophilic proteins’ this means proteins that attract water. As such, often with tendinopathy there can be fairly large swellings at first and the water which gets between the strands in the tendon makes them appear thicker. Anything which happens in this phase tends to be short term.
Tendon Dysrepair
This is the progression of stage 1, it occurs when the initial phase is not sufficiently managed (rested and strengthened appropriately) which allows the tendon to return to it’s original state.
During this phase your bodies attempt to heal the protein causes an increase in proteins which can separate type 1 collagen and relay type 3 collagen which in English means, your body is that co-worker that tries to be helpful and makes the situation worse. This is because type 3 collagen is not as strong or as springy as type 1 collagen. This causes the tendon to become stiffer and less user friendly.
Degenerative tendinopathy
This is the final stage of the continuum and it is believed that much of the damage caused in this stage is irreversible. On the bright side, people in the third phase tend to report less pain but can be at the highest risk of tendon rupture.
How do I know if I’ve got it?
Patellar tendinopathy is characterised by pain at the front of the knee, just downwards from the bottom point of the kneecap. It is often sore to press there and is aggravated by movement which asks a lot of the quads e.g. running, sprinting and in particularly jumping.
So, what do we do about it?
First of all, despite how complicated and scary the bit above sounds, the vast majority of the time you will come to see your physio at stage 1 or 2, as stage 3 takes a really long time or some silly decisions to reach. Physio’s are adept at managing tendinopathies, it is our bread and butter.
The first stage in managing tendinopathies is usually ice and rest. Your GP will often prescribe anti-inflammatories if they are your first port of call which can often be helpful to manage your symptoms. However, studies have shown that prolonged usage of anti-inflammatories can be detrimental to tendon healing. This is thought to be because as you’ve seen above, there’s not a whole lot of inflammation to be found in the tendon by the time you reach phase 2/3.
If you’ve read physio advice and guidance written by us before you will know that I am a fan of self-management of conditions. However, conditions like these it is sensible to seek the advice of one of our physiotherapists at your earliest opportunity.
What can physio do for me?
Biomechanics and progressive loading.
 As always, detailed advice and specific guidance are what you’re looking for with your physiotherapist in a situation like this.
As always, detailed advice and specific guidance are what you’re looking for with your physiotherapist in a situation like this.
At Summit we take a two-pronged attack at managing your tendinopathy. We understand that overload usually comes from some form of biomechanical problem. Therefore, we aim to eliminate the biomechanical problem and to provide a progressive loading program to get you and your problematic tendon back to doing everything you want to.
This is achieved by designing a tailor made exercise program around you and your life, which gets progressively heavier until you feel confident and able to return to your best you.
Extra-corporeal pulse shockwave therapy.
 Shockwave therapy is a treatment method for tendinopathy which is becoming increasingly popular with experts in sports medicine around the world.
Shockwave therapy is a treatment method for tendinopathy which is becoming increasingly popular with experts in sports medicine around the world.
It is now being recommended for various tendinopathies by the National Institute for Health and Clinical Excellence (NICE) these are the people that set the recommendations for clinical excellence used by all registered medical practitioners.
The reason why we use it is if you take the above continuum, many tendinopathies remain in phase 2 for a long period of time, a series of low energy pulse waves through the skin has been shown to be effective in helping tendon problem to return to phase 1. This makes it much easier to manage and to get better.
Hyperbaric Oxygen Therapy (97% oxygen chamber)
 This one is a favourite with our athletes, we all know our bodies need oxygen. More specifically the part of our cells which produce energy known as mitochondria require available oxygen to produce and repair cells. Our chamber is 97% oxygen which floods the body with oxygen allowing a surplus of available oxygen for new cell production. Basically, more oxygen means faster healing.
This one is a favourite with our athletes, we all know our bodies need oxygen. More specifically the part of our cells which produce energy known as mitochondria require available oxygen to produce and repair cells. Our chamber is 97% oxygen which floods the body with oxygen allowing a surplus of available oxygen for new cell production. Basically, more oxygen means faster healing.
We are lucky enough to be able to have experienced exercise clinicians and the ground-breaking tools to provide you the fastest route to getting better should you need us.
Enquire via email to getmebetter@summitphysio.co.uk or by calling 0800 731 2738. Alternatively, book an appointment online today!